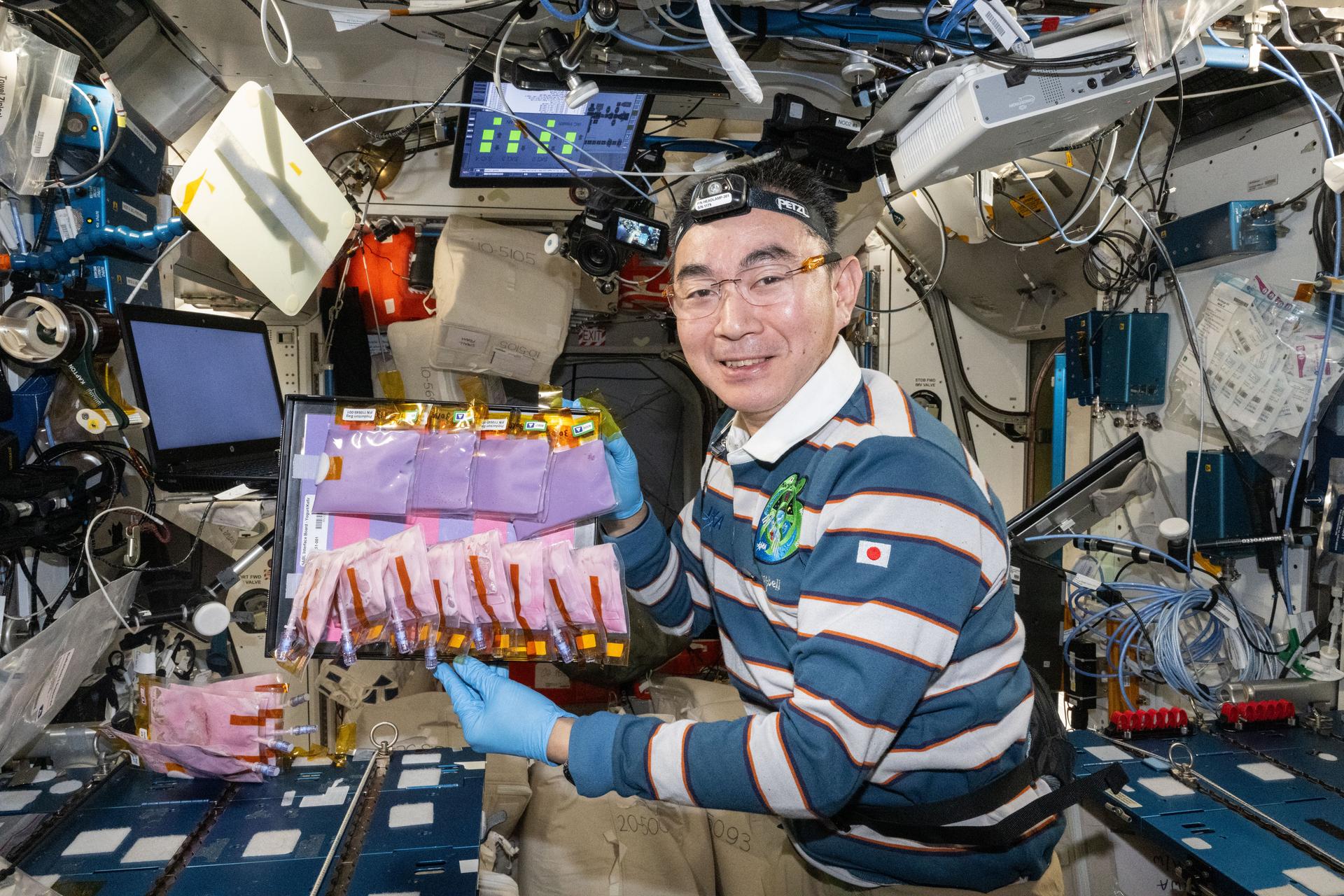
NASA, the National Institutes of Health (NIH), Department of Health and Human Services Biomedical Advanced Research and Development Authority (BARDA), and the Food and Drug Administration (FDA) announce the award of 8 contracts in a multi-agency collaboration that will extend tissue viability and physiological function to a minimum of 6 months using automated engineering capabilities for real-time online readouts in complex human in vitro models, such as tissue chips or microphysiological systems.
The scientific objectives are to better understand 1) disease models, 2) drug development, 3) clinical trial design, 4) chemical and environmental exposures and countermeasures, and 5) physiological changes due to the spaceflight environment. In-depth characterization is a critical next step in the evolution of these technologies is, particularly when considering acute versus chronic exposures.
This effort, sponsored by NASA’s Space Biology Program, reflects a collaboration between NASA’s Science Mission Directorate, NASA’s Human Research Program, NIH’s National Center for Advancing Translational Sciences (NCATS), the NIH National Institute of Allergy and Infectious Diseases (NIAID), the NIH National Cancer Institute (NCI), BARDA, and the FDA. The agencies selected projects that will adapt existing 3D tissues and microphysiological systems (MPS) — also known as “tissue chips” or “organs-on-chips” — to 1) expand tissue viability and robust function for a minimum of 6 months, and 2) fully test and validate these models for acute and chronic stressors.
The selected studies aim to fund the development and validation of tissue chips which can function successfully for 6 months or longer in an automated fashion, to be used for modeling of acute and/or chronic exposures (e.g., to drugs and other compounds, radiation, environmental hazards, infection, microgravity exposure, etc.).
Eight investigators will conduct these investigations from eight institutions in six states. When fully implemented, approximately $16M will be awarded in fiscal years 2022-2025.
Elizabeth Blaber, Rensselaer Polytechnic Institute Understanding the Brain-Liver-Gut Axis during Spaceflight and Aging
Joel Blanchard, ICAHN School of Medicine at Mount Sinai, Identification of Biomarkers and Pathological Mechanisms via Longitudinal Analysis of Neurological and Cerebrovascular Responses to Neurotoxic Stress Using a Multi-cellular Integrated Model of the Human Brain
Guohao Dai, Northeastern University, Bioengineer Long-lasting 3D Neurovascular Microphysiological System to Model Chronic Inflammation-mediated Neurodegeneration
Abhishek Jain, Texas A&M, Long-term Patient iPSC Vessel Chip Model to Assess Stressors of Atherosclerosis and mRNA Therapeutics
Christopher Porada, Wake Forest University, Long-lived Single- and Multi-organ Tissue Equivalent (OTE) Platforms to Model the Response of Human Tissues to Various Stressors
Gordana Vunjak-Novakovic, Columbia University, MORPH: Multi-Organ Repair Post Hypoxia
Joseph Wu, Stanford University, Assessing Long-Term Effects of Radiation Exposure in Engineered Heart & Vascular Tissues
Catherine Yeung, University of Washington, Extended Culture of Kidney MPS and Organoids to Model Acute and Chronic Exposure to Drugs and Environmental Toxins
Related Articles: